Claire’s MND Timeline
With the benefit of hindsight, we believe the first systems of Motor Neurone Disease began in summer 2024, around a year before formal diagnosis in summer 2025. This timeline will be kept updated with two goals: 1. To help others spot the signs of MND as early as possible 2. A practical and efficient way to keep our friends and family updated as the disease progresses.
Claire noticed an imbalance in both her strength and physical appearance during Bodypump classes at the gym, just affecting her left pectoral muscle.
Out of character, Claire began to be susceptible to crying at moments that she would typically handle just fine, both at work and at home. There were no events of laughing at inappropriate times which are sometimes observed with onsite of MND.
Perimenopause was the primary suspect for the change in Claires emotions. HRT options discussed with the decision to take no immediate action as review if no improvement.
While on holiday with friends (and wearing high heel shoes) Claire badly sprained her ankle.
 While on a family summer holiday (and again in high shoes) Claire repeated the same injury
While on a family summer holiday (and again in high shoes) Claire repeated the same injury
Gait issues with the left leg, as expected with following ankle injury. Easing over time, with sporadic stretching and use of ankle support.
We attributed this to secondary issues from walking with an altered gait. Claire had suffered some back pain issues in the past, which were resolved with consistent exercise/gym classes, thus were not surprised with this problem considering the impact the ankle injury had on visiting the gym.
Walking pace decreased, climbing stairs became difficult.
Referral for X-ray of left ankle. Prescription for Naproxen to address back pain and Omeprazole to mitigate the gastrointestinal side effects of continued naproxen use.
Cramping in both legs began, particularly during and after sleep.
Balance significantly impacted. Use of walls and other static object used to reduce risk while moving.
Add Description Here
Add Description Here
X-rays for ankle and left thumb showed no issues.
Significant difficulty participating an gym classes.
MRI showed no issues.
Minor issues/abnormalities observed but no significant finding.
Add Description Here
Following a fall on the way to work Claire made the decision that she was not fit for work.
Prescribed Sertraline for low mood and emotional lability. Reported muscle spasms in left arm.
Results showed no concern although "wear and tear" of nerves noted however inline with age.
Diagnosis of Functional Neurological Disorder (FND). Treatment advised include yoga, meditation, social engagement and replacing Sertraline with Duloxetine. MRI of spine and brain advised to be sure of no issue however unlikely to show anything.
Add Description Here
Complete at Tees Valley Hospital.
Stated brain MRI "fine"
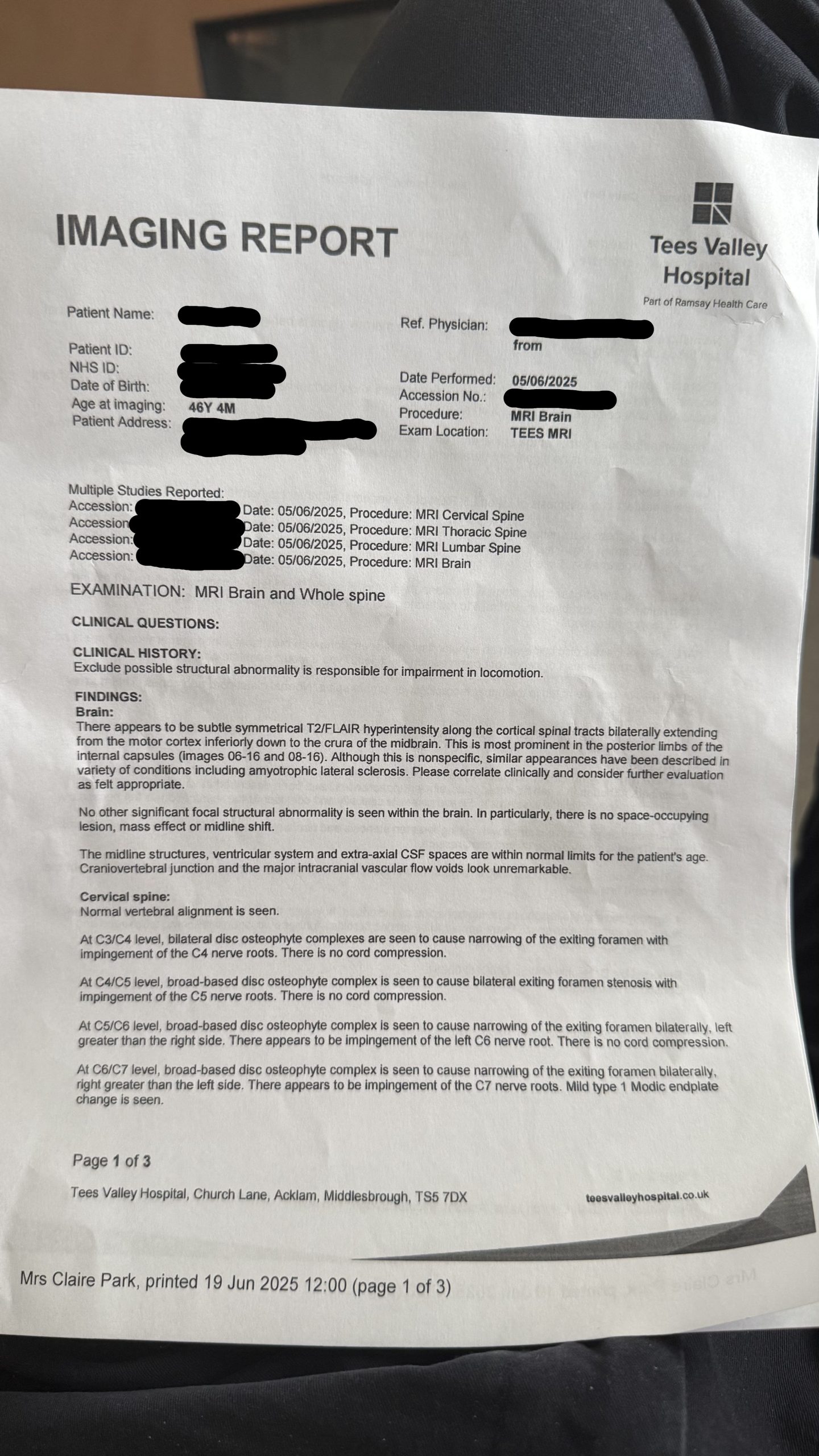
Key Phrases Explained:
• “Subtle symmetrical T2/FLAIR hyperintensity”:
On MRI, this means there are areas in the brain that appear brighter than usual (hyperintense) on specific sequences (T2/FLAIR). These sequences are particularly good at detecting abnormalities like inflammation, demyelination, or gliosis (scarring).
• “Along the corticospinal tracts bilaterally”:
These tracts are major pathways that carry movement-related signals from the brain’s motor cortex to the spinal cord. Bilateral means it’s affecting both sides.
• “Extending from the motor cortex inferiorly down to the crura of the midbrain”:
The changes are seen starting at the motor control area of the brain and following the pathway downward through the brainstem.
• “Most prominent in the posterior limbs of the internal capsules”:
This region is a key transit point for the corticospinal tracts. It’s more affected or brighter here on the images noted.
• “Although this is nonspecific…”:
The finding is not unique to one disease. It could occur in several conditions, some of which are serious, some not.
• “Similar appearances have been described in… amyotrophic lateral sclerosis (ALS)”:
The pattern of brightness along the motor pathways can be seen in ALS, a progressive motor neuron disease. However, this is not a diagnosis, just an observation that matches patterns sometimes seen in ALS.
• “Please correlate clinically and consider further evaluation”:
The radiologist is saying: “This could be significant, but we can’t say for sure from the scan alone. The doctor should evaluate the patient’s symptoms and clinical history to decide if more testing is needed.”
⸻
Bottom Line:
This MRI shows subtle abnormalities along the brain’s motor pathways. These can be seen in conditions like ALS, but they’re not diagnostic on their own. Clinical symptoms (like muscle weakness, twitching, or stiffness) and possibly further tests (e.g., EMG, neurological exams) are needed to understand what this means for the individual.
Noted muscule spasms in all limbs. Confused by clear nerve conduction results despite MRI findings suggesting ALS. Recommended admission for further tests in London. We requested a call to the on-call neurologist at South Tees hospital due to a preference of testing locally. Call between private and NHS neurologists completed while we observed via e-consultation.
On call neurologists called approximately 30 mins later and advised a bed is expected at 18:00. Attended South Tees and completed an inital physical exam by neurologist who stated he was confident in a diagnosis of MND.
Repeated nerve conduction test. Lung function test. Blood gas test.
Formal diagnosis of MND given. Prescribed Riluzole is the only licensed medication in the UK that has shown a survival benefit for people with Motor Neurone Disease (MND). It's not a cure, but it may slow down the progression of the disease. Other medications are used to manage specific symptoms of MND, such as muscle stiffness, cramps, drooling, and breathlessness.